Have you ever felt a “gut-wrenching” sensation during moments of stress or anxiety? This isn’t just a figure of speech; it’s a reflection of the profound connection between our emotional experiences and digestive health. Emerging research reveals that trauma can significantly impact gut health, leading to a cascade of physical and psychological effects. In this article, we’ll delve deep into the intricate relationship between trauma and gut health, exploring how past experiences shape our digestive system and overall well-being.
Table of Contents
The Gut-Brain Axis – A Two-Way Street
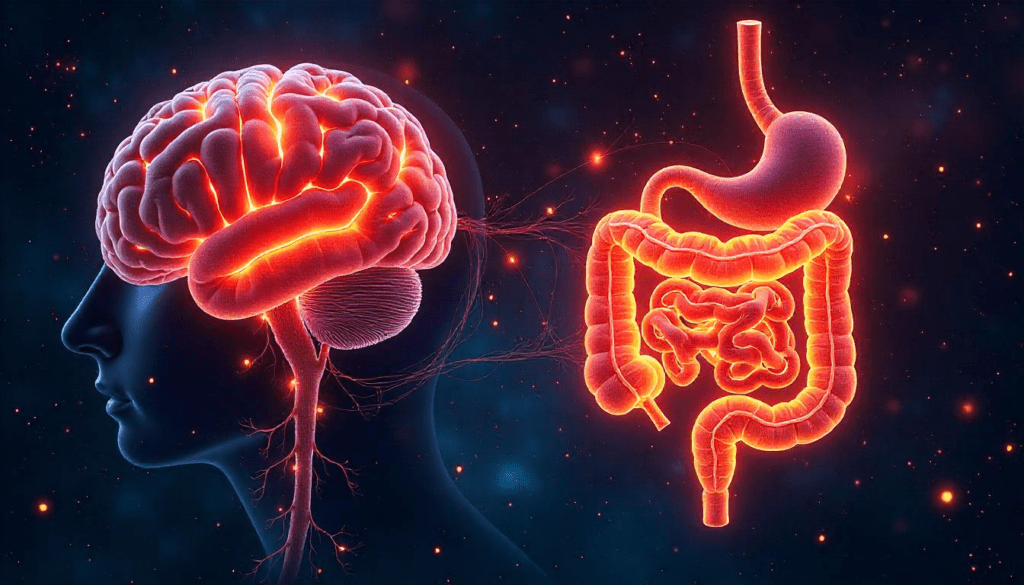
The gut-brain axis is a complex communication network linking the central nervous system (CNS) and the enteric nervous system (ENS) of the gastrointestinal tract. This bidirectional pathway involves neural, hormonal, and immunological signaling, allowing the brain and gut to influence each other’s functions.
Key Components:
- Vagus Nerve: The primary neural pathway facilitating communication between the gut and brain.
- Neurotransmitters: Chemicals like serotonin and dopamine are produced in the gut and influence mood and cognition. Trillions of microorganisms residing in the gut play a role in immune function and neurotransmitter production.
- Microbiota: Trillions of microorganisms residing in the gut play a role in immune function and neurotransmitter production.
Understanding this axis is crucial, as disruptions can lead to both gastrointestinal and psychological disorders.
How Trauma Disrupts Digestive Health

Trauma doesn’t just leave emotional scars — it can fundamentally alter how your body functions, especially your digestive system. Whether it stems from childhood neglect, abuse, combat, loss, or even long-term emotional stress, trauma creates a lasting imprint on the body, particularly the gut-brain connection.
Trauma and the Fight-or-Flight Response
When we experience trauma, the body activates its fight-or-flight mode, a survival mechanism driven by the autonomic nervous system, specifically the sympathetic branch. This response increases heart rate, redirects blood flow to muscles, and shuts down “non-essential” functions — like digestion.
In a healthy individual, this stress response is temporary. But for trauma survivors, the stress often becomes chronic, keeping the body in a constant state of alertness. Over time, this dysregulation takes a toll on the gastrointestinal system.
Common Gut-Related Symptoms of Trauma
Many people don’t immediately associate their digestive symptoms with past emotional wounds, but the link is strong. Trauma can contribute to:
- Irritable Bowel Syndrome (IBS): One of the most well-documented conditions linked to trauma. People with IBS are significantly more likely to have a history of trauma or PTSD. Symptoms include chronic abdominal pain, cramping, bloating, gas, diarrhea, and/or constipation.
- Functional Dyspepsia: A condition marked by a feeling of fullness, discomfort, or nausea, especially after eating — often seen in those with anxiety or unresolved trauma.
- Leaky Gut Syndrome: Trauma increases inflammation, which can weaken the intestinal lining. This makes the gut more permeable, allowing toxins, undigested food, and bacteria to “leak” into the bloodstream, triggering immune reactions and further inflammation.
- Appetite Dysregulation: Some people develop hyperphagia (overeating) as a coping mechanism, while others lose their appetite entirely. Both patterns disrupt digestion and nutrient absorption.
- Dysbiosis (Microbiome Imbalance): Trauma alters the microbial composition of the gut. Stress hormones like cortisol can reduce beneficial bacteria such as Lactobacillus and Bifidobacterium, and allow overgrowth of harmful species like Candida or certain Clostridium strains.
Trauma and Gut Motility
When the nervous system is dysregulated due to trauma, the gut muscles that move food through the digestive tract can become either hyperactive (leading to diarrhea) or hypoactive (causing constipation). This is why people with trauma histories often swing between extremes — some constantly feel “on edge” with a nervous stomach, while others feel sluggish and bloated.
The Vicious Cycle: Gut Health Fuels Mental Health
What makes trauma and gut health so intricately linked is that it’s not a one-way street. Just as trauma can cause gut issues, poor gut health exacerbates mental health problems.
When your gut is inflamed or imbalanced:
- Your brain receives inflammatory signals that can worsen anxiety, depression, or PTSD.
- Neurotransmitter production is disrupted — especially serotonin, about 90% of which is made in the gut.
- You may feel foggy, irritable, or emotionally reactive — even when you’re not “actively” thinking about the traumatic event.
The Role of the Microbiome in Mental Health

You’ve probably heard the term “gut feeling” before — but what if your gut is actually thinking with you? It’s not just a metaphor. The gut is now often referred to as the “second brain,” and for good reason: the vast network of neurons in the gut, combined with the trillions of microbes that live there, play a direct role in your mental health.
What Is the Microbiome?
Your gut microbiome is made up of over 100 trillion microorganisms — including bacteria, viruses, fungi, and protozoa — that live in your gastrointestinal tract. This living ecosystem weighs about three pounds, rivals the number of cells in your entire body, and communicates directly with your brain via the gut-brain axis.
These microbes are responsible for:
- Digesting food
- Producing vitamins (like B12, K)
- Modulating the immune system
- Regulating inflammation
- Producing neurotransmitters that affect your mood
When the balance of good and bad bacteria in the gut is disturbed — a condition known as dysbiosis — it can directly contribute to mental health problems.
The Microbiome’s Role in Trauma and PTSD
Scientific studies are increasingly showing that people with trauma-related conditions — especially Post-Traumatic Stress Disorder (PTSD) — often show signs of gut microbiome disruption.
Several key findings:
- Individuals with PTSD have less microbial diversity, meaning fewer types of good bacteria and more overgrowth of harmful ones.
- They often have lower levels of Lactobacillus and Bifidobacterium, strains known to reduce anxiety and support the immune system.
- Trauma is also linked to increased levels of pro-inflammatory bacteria, which can elevate systemic inflammation and disrupt brain function.
One landmark study even found that trauma-induced stress in early childhood can permanently alter the microbiome, increasing the risk of depression and anxiety later in life.
Neurotransmitter Production: It Starts in the Gut
Did you know that nearly 90% of your serotonin — the “feel-good” chemical — is produced in your gut?
- Serotonin affects mood, sleep, and appetite.
- Dopamine, often associated with motivation and pleasure, is also produced in the gut.
- GABA (gamma-aminobutyric acid), which helps calm anxiety, is influenced by gut bacteria.
When your microbiome is out of balance due to trauma, poor diet, antibiotics, or chronic stress, the production and signaling of these mood-related chemicals break down — resulting in symptoms like irritability, mood swings, and emotional numbness.
Inflammation: The Silent Link
An unhealthy microbiome contributes to chronic low-grade inflammation, which is now recognized as a major factor in depression, anxiety, and cognitive dysfunction. This inflammation can:
- Disrupt the blood-brain barrier
- Reduce neuroplasticity (your brain’s ability to adapt and heal)
- Amplify trauma-related symptoms
In short, your gut bugs may be small, but they have a massive say in how you feel — and how well you recover from psychological wounds.
Microbiome and Cognitive Function
Recent research also links gut health to cognitive performance. People with a more diverse gut microbiome perform better on memory, attention, and emotional regulation tasks. This is crucial for trauma survivors, as trauma often impairs focus, clarity, and emotional processing.
Inflammation, Leaky Gut, and Autoimmune Responses
You might not think your gut has anything to do with your joint pain, chronic fatigue, or brain fog — but if you’ve experienced trauma, your gut may be ground zero for a cascade of inflammatory and autoimmune responses.
Trauma, especially when it becomes chronic or unresolved, can wreak havoc on your immune system through a phenomenon called gut permeability, more commonly known as leaky gut syndrome. And when the gut wall starts to break down, inflammation isn’t far behind.
What Is Leaky Gut?
The lining of your intestines is like a fine mesh — designed to absorb nutrients but keep harmful substances like pathogens, toxins, and undigested food particles out of your bloodstream. When trauma and chronic stress disrupt this barrier, it becomes more permeable. This condition is what people refer to as “leaky gut.”
Think of it like a coffee filter tearing — suddenly the grounds are seeping into your cup.
When the gut barrier is compromised:
- Toxins and bacteria “leak” into the bloodstream
- The immune system perceives them as threats
- Systemic inflammation is triggered
- Over time, this can lead to autoimmune diseases
Trauma and the Inflammatory Cascade
Unresolved trauma activates the hypothalamic-pituitary-adrenal (HPA) axis, which leads to sustained high levels of cortisol — your body’s primary stress hormone. While cortisol is helpful in acute stress situations, too much for too long wears down your immune defenses.
What happens next?
- The body remains in a pro-inflammatory state
- Inflammatory molecules like cytokines flood your system
- These molecules don’t just stay in the gut — they can travel to the brain, joints, and organs
This is why so many people with trauma histories report a wide range of seemingly unrelated symptoms, such as:
- Skin issues (eczema, psoriasis)
- Joint pain and stiffness
- Hormonal imbalances
- Brain fog
- Chronic fatigue
- Frequent infections
The Gut-Immune Connection
The gut houses about 70% of your immune system. So when your gut health is compromised by stress, trauma, or dysbiosis, your immune system becomes confused. It may begin attacking not just invading microbes but your own body’s tissues — a hallmark of autoimmune disease.
Autoimmune disorders that have been linked to trauma and gut imbalance include:
- Rheumatoid Arthritis
- Celiac Disease
- Hashimoto’s Thyroiditis
- Lupus
- Type 1 Diabetes
These conditions often emerge or flare up after a major stressor or traumatic event, even years after the original trauma.
Inflammation and Mental Health
The relationship between gut inflammation and mental health is a two-way street. Not only does trauma-induced inflammation affect your physical body, but it also:
- Interferes with neurotransmitter production
- Damages the blood-brain barrier
- Impairs emotional regulation
- Increases risk of depression, anxiety, and PTSD
That’s why many people feel “emotionally inflamed” — on edge, irritable, overly reactive — even when nothing seems to be wrong externally. The inflammation inside is speaking.
Strategies for Healing the Gut-Brain Connection
The good news? While trauma may leave lasting marks on the gut and brain, healing is absolutely possible. It requires a holistic, trauma-informed approach that nurtures both emotional and physical well-being. By repairing the gut-brain axis, you not only improve digestion — you unlock a better mood, stronger immunity, and a deeper sense of inner calm.
Below are evidence-based, gut-friendly strategies designed to support recovery from trauma and restore digestive harmony.
1. Trauma-Informed Therapy
Mental healing is physical healing — especially when it comes to the gut-brain connection.
Effective therapies that address trauma at its root:
- EMDR (Eye Movement Desensitization and Reprocessing): Proven effective for PTSD, EMDR helps rewire traumatic memories stored in the nervous system.
- Somatic Experiencing: Focuses on body awareness to release trauma trapped in the body — ideal for those with gut tension or chronic pain.
- Internal Family Systems (IFS): Helps people understand and integrate “parts” of themselves stuck in trauma, often reducing anxiety-related digestive symptoms.
- Trauma-focused CBT (Cognitive Behavioral Therapy): Especially helpful for identifying gut-related triggers tied to anxiety or fear.
2. Anti-Inflammatory & Gut-Healing Nutrition

What you eat profoundly affects your microbiome, inflammation levels, and even your mental clarity.
Gut-friendly, trauma-reducing foods:
- Bone broth – rich in collagen and amino acids that repair the gut lining.
- Fermented foods – like kimchi, sauerkraut, kefir, and yogurt introduce beneficial probiotics.
- Omega-3 fats – found in salmon, flaxseed, and walnuts, help lower inflammation.
- Leafy greens & cruciferous vegetables – detoxifying and rich in antioxidants.
- Turmeric & ginger – powerful anti-inflammatory spices with gut-soothing effects.
Foods to minimize:
- Ultra-processed foods
- Refined sugars
- Alcohol
- Gluten (if sensitive)
- Industrial seed oils (canola, soybean)
3. Probiotics and Prebiotics
Your gut bacteria are your allies in healing. After trauma, the microbiome often becomes imbalanced — and supplementing with probiotics and prebiotics can help restore harmony.
- Probiotics (beneficial bacteria): Look for strains like Lactobacillus rhamnosus, Bifidobacterium longum, and Saccharomyces boulardii — all known to support gut and mental health.
- Prebiotics (fibers that feed probiotics): Found in onions, garlic, bananas, chicory root, asparagus, and oats.
4. Mind-Body Practices That Calm the Gut
Stress shrinks the diversity of your microbiome and increases gut inflammation. Mind-body practices help rebalance your nervous system, allowing digestion to resume its natural rhythm.
- Breathwork: Deep belly breathing stimulates the vagus nerve, which regulates digestion and mood.
- Yoga: Gentle movements like twists and forward folds enhance gut motility and reduce tension.
- Meditation & mindfulness: Helps detach from the constant “fight-or-flight” loop and fosters gut-brain awareness.
- Progressive muscle relaxation: Calms the enteric nervous system, relieving tension held in the abdominal region.
5. Supplemental Support for Gut & Nervous System Repair
Supplements can speed up healing — especially when trauma has caused nutrient depletion or inflammation.
Targeted supplements:
- L-Glutamine: Supports gut lining repair.
- Magnesium glycinate: Calms the nervous system and helps with constipation.
- Zinc carnosine: Promotes gut mucosal healing.
- Vitamin D: Modulates immunity and gut barrier integrity.
- Ashwagandha or Rhodiola: Adaptogens that lower cortisol and reduce gut inflammation.
6. Sleep, Circadian Rhythm & Gut Health
Trauma often disrupts sleep patterns, and poor sleep is one of the fastest ways to destroy gut health. The gut and brain run on circadian rhythms — internal clocks that regulate everything from digestion to hormone production.
To restore your rhythm:
- Stick to consistent bed and wake times
- Limit screen exposure before bed
- Eat dinner at least 2–3 hours before sleep
- Consider melatonin or magnesium for temporary support
7. Nature, Movement, and Emotional Release
The trauma-gut connection thrives on movement and grounding.
- Daily walks in nature reduce cortisol and enhance gut microbial diversity.
- Dancing, shaking, or even crying are powerful emotional releases that support nervous system regulation.
- Cold exposure (like cold showers) can tone the vagus nerve and lower gut inflammation.
Final Thoughts: Start Small, Heal Big
Healing the gut-brain connection after trauma isn’t about being perfect — it’s about being consistent and kind to yourself. Whether you start with just one probiotic capsule, five minutes of deep breathing, or a single therapy session, you are already breaking the trauma-inflammation cycle.
There is no “one-size-fits-all” in trauma recovery — but when you treat your gut with love, your brain feels the difference.
Note: This blog post is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional for personalized recommendations.
Frequently Asked Questions (FAQs)
1. Can trauma really affect your gut health?
Yes, trauma can significantly impact your gut health. Chronic or unresolved trauma activates the body’s stress response, leading to inflammation, changes in gut motility, and an imbalance in gut bacteria. This disruption in the gut-brain axis can cause digestive issues like bloating, IBS, constipation, or diarrhea.
2. What are the symptoms of trauma stored in the gut?
Common gut-related symptoms of unresolved trauma include:
- Chronic bloating or gas
- Irritable Bowel Syndrome (IBS)
- Constipation or diarrhea
- Food sensitivities
- Abdominal pain or tightness
- Loss of appetite or emotional eating
- Fatigue and brain fog
These symptoms often persist even when conventional GI tests come back “normal.”
3. How does trauma cause leaky gut?
Trauma increases cortisol and inflammatory cytokines, which weaken the gut lining. This allows toxins and undigested food particles to enter the bloodstream — a condition known as leaky gut. The immune system reacts to these invaders, leading to widespread inflammation and sometimes autoimmune responses.
4. What is the gut-brain axis and why is it important in trauma recovery?
The gut-brain axis is the two-way communication system between your gastrointestinal system and central nervous system. Trauma can dysregulate this axis, impairing digestion, mood regulation, and immune responses. Healing the gut helps regulate emotional responses and supports trauma recovery on a physical level.
5. Which probiotics are best for healing trauma-related gut issues?
Probiotic strains that may help include:
- Lactobacillus rhamnosus: Reduces anxiety
- Bifidobacterium longum: Supports gut-brain signaling
- Saccharomyces boulardii: Helps repair the gut lining and prevent inflammation
Choose a multi-strain probiotic with at least 10–20 billion CFU and consult a healthcare provider for personalized recommendations.
