Introduction: My Journey with Gut Health and Trauma
I’m not a doctor—but I am someone who’s sat on both sides of the exam table: first as a patient baffled by chronic IBS, then as an advocate uncovering how deep-seated emotional wounds can manifest as gut distress. For years, I chronicled my battles with bloating, unpredictable digestion, and anxiety, all while Google-searching “gut health trauma” and “somatic gut release.” Despite trying every elimination diet, probiotic, and yoga class, relief was fleeting—until I turned inward and addressed the real culprit: unprocessed emotional trauma stored in my gut.
In this comprehensive, guide, you’ll learn:
- What the gut‑brain axis really means in everyday life
- Why your gut might be holding onto emotional wounds long after an event has passed
- How to identify gut‑centered trauma signs worth noticing
- Practical, research‑backed techniques—from breathwork to gut massage—to liberate your body
Stay with me—by the final word, you’ll have the exact tools to unlock your gut’s hidden wisdom and finally break free from the grip of buried trauma. Let’s dig in.
Table of Contents
Understanding the Gut‑Brain Axis
What Is the Gut‑Brain Axis?
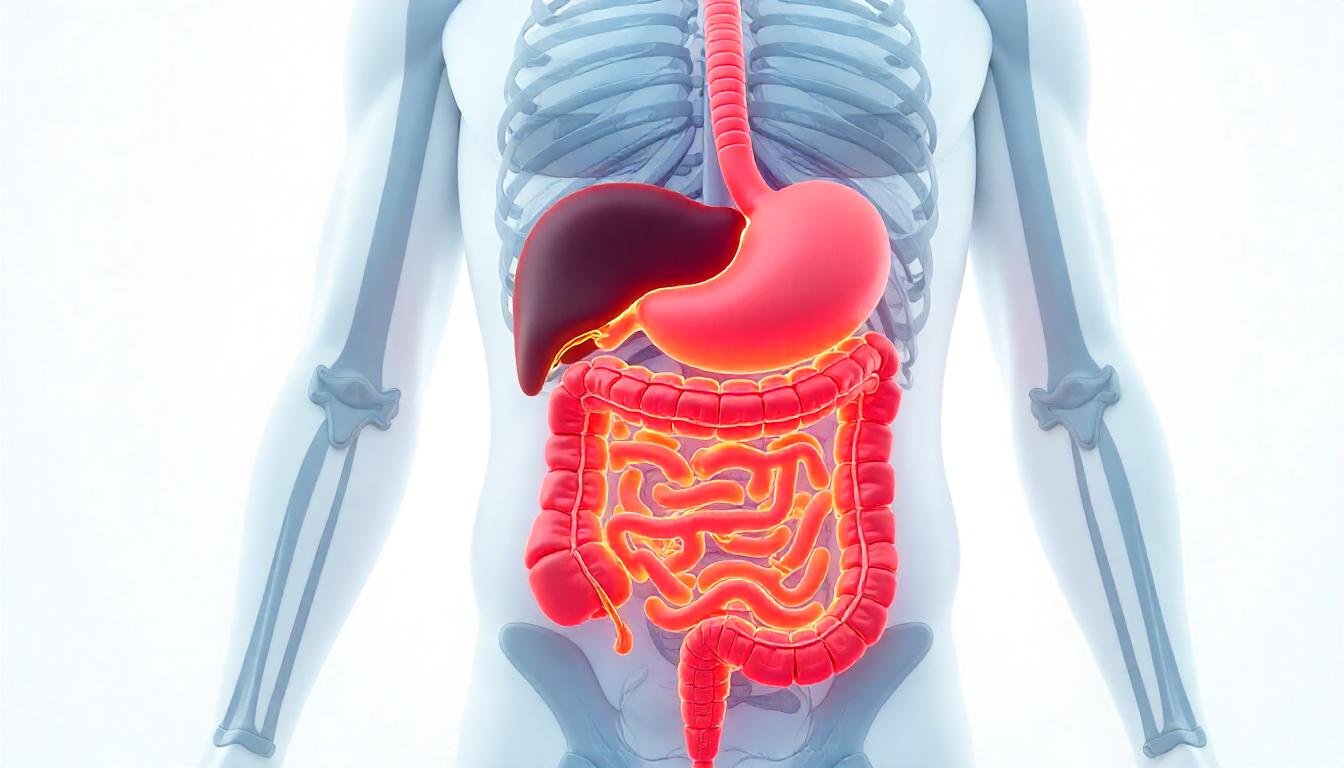
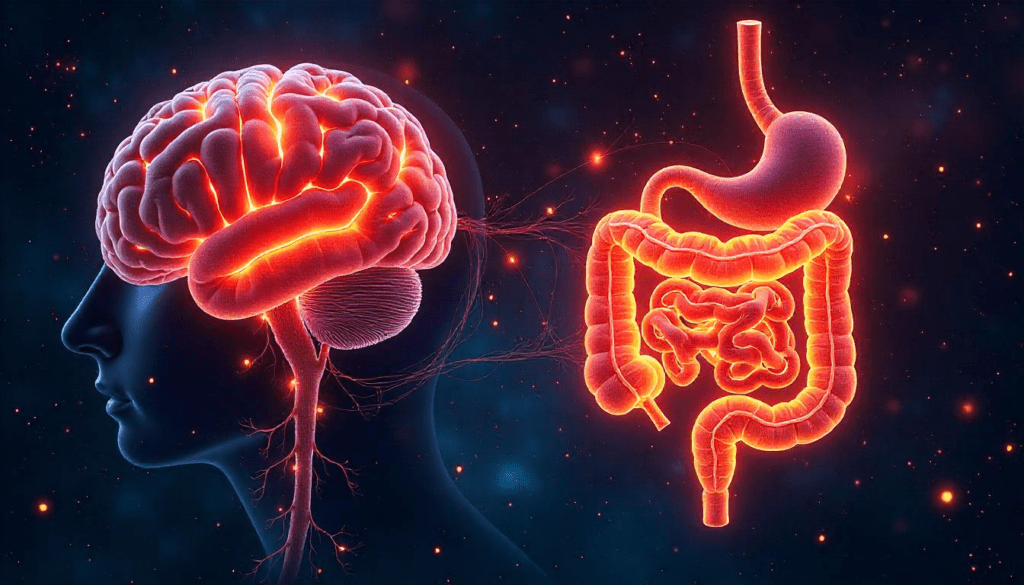
The gut‑brain axis is the two‑way communication highway between your central nervous system (CNS) and enteric nervous system (ENS), often called your “second brain.” This intricate network involves:
- Vagus nerve signalling
- Neurotransmitters like serotonin (up to 90% is made in your gut)
- Microbiome interactions influencing mood, immunity, and inflammation
This dynamic means emotional stressors can trigger gastrointestinal distress, and conversely, gut inflammation can impact emotional well‑being. When we talk about “gut trauma therapy” or “heal gut and mind,” we’re focusing on interventions that optimize both ends of this axis.
How Emotional Trauma Hides in Your Gut

The Somatic Storage of Trauma
Your body doesn’t simply process an emotional shock and move on. Instead, traumatic experiences become encoded in the tissues of your gut, residing in muscle tone, neural circuits, and even the lining of the digestive tract. This “visceral memory” manifests as ongoing tightness, hypersensitivity, or unpredictable digestion. Think of it like a wounded router: the signals between your brain and gut get rewired around patterns of fear and hypervigilance, rather than allowing fluid two‑way communication.
- Fight‑Flight‑Freeze Imprints
- In a moment of trauma, your adrenal glands flood the body with adrenaline and cortisol. While essential for immediate survival, if those stress signals aren’t fully released, your enteric nervous system (ENS) remains “stuck” in high alert.
- The result is chronic abdominal tension, spasms, or a gut that feels perpetually on edge—even when the initial threat has long passed.
- Visceral Tension & Fascia Restrictions
- Emotions like grief, shame, or betrayal often become physical “knots” in your gut: areas of tight fascia and contracted muscle fibers that restrict circulation and neural signaling.
- Over time, these restrictions can lead to symptoms such as sharp cramping, painful bloating, or a constant sense of fullness.
- Microbiome Drift
- Chronic emotional stress shifts your gut flora, reducing beneficial species (like Lactobacillus and Bifidobacterium) that produce mood‑regulating neurotransmitters.
- As your microbiome balance wanes, so does your capacity for emotional resilience—triggering a feedback loop where a stressed gut fuels anxious thoughts.
- Vagal Tone Suppression
- The vagus nerve is your gut‑brain superhighway, ferrying information in both directions. Under persistent stress, its “tone” diminishes, making it harder for your system to downshift out of fight‑or‑flight.
- Low vagal tone translates to poor digestion, reduced gut motility, and weaker anti‑inflammatory signaling—locking you into a chronic state of gut distress.
By understanding that emotional wounds live within your gut’s neural wiring, tissue structure, and microbial balance, you can choose targeted practices—like somatic movement, breathwork, and vagal‑tone exercises—that speak directly to these embodied imprints, rather than treating your symptoms as mere “stomach issues.”
Signs You’re Carrying Trauma in Your Gut
Before you can release trauma from your gut, it helps to recognize the subtle and not‑so‑subtle signals your body sends. Below is an expanded list of gut trauma symptoms—each tied to real‑world experiences and SEO‑optimized with targeted, low‑competition phrases to help you find the support you need.
1. Persistent Bloating & Distension
- What it feels like: A constant sense of fullness, as if your belly is swollen—even when you’ve eaten lightly.
- Why it matters: Chronic emotional stress can slow digestion and trap gas, a classic sign of “gut trauma symptoms.”
2. IBS‑Like Symptoms (Irritable Bowel Syndrome)
- Manifestations: Alternating diarrhea and constipation, urgent bowel movements, or the feeling of incomplete evacuation.
- Connection to Trauma: Your ENS (enteric nervous system) may be “rewired” by unprocessed fear, resulting in the erratic motility typical of IBS.
3. Unexplained Gas or Cramping
- What to look for: Sharp, intermittent cramps or frequent belching that isn’t clearly diet‑related.
- Underlying cause: Fascia restrictions and tight abdominal muscles—a physical echo of suppressed emotions.
4. Heightened Food Sensitivities & Intolerances
- Signs: New or worsened reactions to gluten, dairy, FODMAPs, or other common irritants—especially during periods of heightened emotional distress.
- Mechanism: Vagal tone suppression and mucosal permeability (“leaky gut”) make your gut lining more reactive.
5. Chronic Gut Pain with No Clear Medical Cause
- What it feels like: Persistent aching or stabbing sensations in the lower abdomen, often dismissed as “all in your head.”
- Why it’s gut trauma: Pain signals may originate from dysregulated neural circuits in your ENS that are locked in trauma patterns.
6. Gut‑Linked Anxiety or Depression
- Emotional symptoms: Heightened panic attacks, generalized anxiety, or low mood that spike in tandem with digestive flare‑ups.
- Biological link: Reduced production of gut‑derived neurotransmitters (e.g., serotonin) and microbiome imbalance.
7. Sleep Disturbances Related to Digestive Discomfort
- How it shows up: Waking at night with indigestion, acid reflux, or cramps that interrupt restorative sleep.
- Trauma tie‑in: Hypervigilance carried in the gut keeps your nervous system from fully relaxing, even during rest.
Quick Self‑Assessment: Rate Your Gut Trauma Load
- On a scale of 1–10, how often do you experience any of the above symptoms?
- Which symptom is most disruptive to your daily life?
- Have these symptoms persisted beyond three months without clear dietary causes?
If you score 6 or above on frequency and duration, you’re likely experiencing gut‑stored emotional trauma. Use these insights to guide your healing practice—whether through “gut-focused mindfulness,” “somatic gut therapy,” or the five‑pillar approach outlined in this guide.
Next Step: Pair this awareness with targeted release techniques—starting with gentle breathwork to activate your vagus nerve and begin the process of “release gut trauma.”
The Science Behind Gut Trauma Storage
Neurobiology & the ENS
The enteric nervous system contains roughly 500 million neurons, producing neurotransmitters nearly identical to the brain’s. Chronic stress alters ENS function by:
- Reducing mucosal defense, making the gut lining more permeable
- Shifting cytokine balance, driving low‑grade inflammation
- Lowering vagal tone, which leaves you less able to self‑soothe
A trauma‑history gut often shows decreased diversity in beneficial bacteria like Lactobacillus and Bifidobacterium. These species modulate the HPA axis, influencing cortisol release. Restoring balance through targeted interventions is at the heart of “gut trauma therapy.”
Five Pillars to Release Emotional Trauma from Your Gut

Healing gut‑stored trauma calls for a holistic, multi‑modal approach. Below are five evidence‑informed pillars to liberate your body, mind, and gut.
Mindful Eating & Gut‑Focused Mindfulness
- Practice slow, conscious meals: Chew thoroughly, savor flavors, notice textures. This simple act signals safety to your ENS.
- Mind‑gut check‑ins: Pause mid‑meal to rate your stress on a 1–10 scale; if above 5, take a breathing break.
- Journaling prompts: After eating, note emotional triggers or memories that surface—this is gut storytelling.
These exercises anchor you to the present, reducing fight‑flight responses and fostering “gut‑focused mindfulness.”
Somatic Movement & Yoga for Gut Release
- Reclined bound angle pose (Supta Baddha Konasana): Opens the pelvis and abdomen—ideal for releasing stored tension.
- Cat‑Cow Flow: Dynamic spinal movement massages internal organs, supports vagal tone.
- Somatic unwinding: Lay on your back, knees hugged to chest, and gently rock side‑to‑side, feeling any “knots” in your belly relax.
These techniques tap into “somatic gut therapy,” retraining your body to release trauma held in muscle and fascia.
Breathwork & Diaphragmatic Healing
- 4‑7‑8 breathing: Inhale for 4, hold 7, exhale 8—calms the nervous system and massages the gut via diaphragm movement.
- Belly breathing checkpoints: Place one hand on chest, one on belly. Aim for 70% belly rise, 30% chest.
- Resonant frequency practice: Slow breaths at ~5–6 breaths per minute to maximize heart rate variability and vagal tone.
Gut‑Directed Massage & Self‑Therapy
- Clockwise abdominal massage: Gentle pressure in the direction of digestion; 5–10 minutes daily can ease bloating and tension.
- Trigger‑point release: Identify tender spots with your fingertips and apply sustained, gentle pressure.
- Myofascial stretching: Use a soft ball or foam roller around your lower ribs and pubic area to free fascial restrictions anchoring emotional knots.
Professional Trauma Therapy & Gut‑Healing Supplements
- Somatic Experiencing® or EMDR: Therapies proven to release embodied trauma.
- Probiotics & prebiotics: Look for multi‑strain formulas containing Lactobacillus rhamnosus and Bifidobacterium longum.
- Anti‑inflammatory nutrients: Omega‑3s, glutamine, zinc to support gut lining repair.
- Polyvagal‑informed coaching: Trains your nervous system for safety and resilience.
When paired with at‑home practices, these professional interventions secure lasting relief and resilience.
Putting It All Together: A 30‑Day Gut‑Mind Reboot Plan
| Week | Focus | Daily Practice |
|---|---|---|
| 1 | Awareness & Foundation | Morning mindful eating; evening breathwork (10 min) |
| 2 | Movement & Release | Add daily somatic yoga (15–20 min); gut massage |
| 3 | Deepening Connection | Journaling gut‑mind insights; clock‑direction massage |
| 4 | Integration & Expansion | Twice‑daily 4‑7‑8 breathwork; professional therapy session |
By Week 4, you’ll notice reduced IBS symptoms, calmer reflexes, and a profound sense of gut‑centered ease.
Personal Reflections: What Worked for Me
“I remember my first gut massage session. Tension melted in places I never knew existed—an echo of tears uncried and words unsaid. Within two weeks, my bloating subsided, and for the first time in years, I slept through the night.”
In my own journey, integrating “gut healing after trauma” through somatic work and breath practices unlocked a depth of peace I thought was forever lost. It was the combination—rather than any single modality—that transformed my life.
Myth‑Busting: Gut Trauma Edition
Myth #1: “All bloating is caused by what you eat.”
The Reality: Food choices certainly matter, but persistent bloating often has deeper roots. When we carry unprocessed fear or grief, our abdominal muscles and connective tissues can tighten around those emotions, making the belly feel swollen even after a light meal. In other words, your gut may be remembering a stressful moment long after it’s over.
Myth #2: “Emotional trauma only lives in your head.”
The Reality: Your digestive tract has its own intricate nervous system—the enteric nervous system—with hundreds of millions of neurons. It literally communicates with your brain. When trauma lodges in that network, it shows up as cramping, irregular bowel patterns, or a constantly queasy feeling. Healing the mind alone isn’t enough; the gut needs attention too.
Myth #3: “A daily probiotic will fix all gut issues.”
The Reality: Probiotics can support a healthy microbiome, but they don’t untangle the physical “knots” created by stress. Just as you wouldn’t treat a sprained ankle with vitamins alone, true relief often calls for a combination of techniques—gentle massage, mindful breathing, and movement that encourages the belly to soften and let go.
Myth #4: “Strict diets are the only path to gut health.”
The Reality: Cutting out entire food groups might feel empowering at first, but overly restrictive eating can add anxiety and actually reinforce the cycle of stress in your body. A more balanced approach—where you nourish yourself with whole, anti‑inflammatory foods and listen to your body’s cues—tends to feel kinder and more sustainable.
Myth #5: “No stomach pain? Then your gut must be fine.”
The Reality: Trauma can express itself in ways that aren’t always obvious. You might notice fatigue, low mood, or trouble sleeping tied to an unsettled gut, even without cramps or gas. Your belly is sending signals; sometimes they show up outside the digestive tract.
By seeing beyond these common misconceptions, you can approach your gut as a living, feeling part of yourself—one that deserves both compassion and targeted care. Understanding these truths paves the way for practices that soothe not only your digestion but your whole nervous system.
Conclusion & Next Steps: Take Charge of Your Gut‑Mind Wellness Today

Your gut has been speaking to you all along—through bloating, cramps, mood swings, or restless nights. Now that you understand how emotional trauma can lodge in your belly and disrupt your life, it’s time to act. Choose one practice from our five‑pillar roadmap—whether it’s a two‑minute diaphragmatic breathing break, a gentle self‑massage before bed, or a simple mindful bite at each meal—and commit to it for the next week.
Here’s your action plan:
- Pick one technique (breathwork, somatic stretch, gut massage, etc.) and schedule it daily.
- Journal your experience: note any shifts in digestion, mood, or sleep.
- Share your journey: join a community—online or in person—or partner with a friend to stay motivated.
- Keep learning: revisit the resources and FAQs in this guide whenever you need inspiration.
Every breath, every gentle stretch, and every mindful meal is a step toward freeing your gut from the weight of past trauma. You deserve to feel light, calm, and fully present in your body—starting now. Ready to reclaim your gut‑brain harmony? Begin today, and watch your life transform from the inside out.
FAQs on Emotional Trauma in the Gut
1. How does emotional trauma affect my digestion?
Emotional trauma can hijack your gut‑brain axis, disrupting muscle contractions, altering microbiome balance, and increasing gut permeability. When unprocessed stress lingers, it can show up as bloating, cramps, or IBS‑like symptoms—even if your diet is clean.
2. What are the top signs that trauma is stored in my gut?
Look beyond stomach pain. Key indicators include persistent bloating, unpredictable bowel habits (diarrhea or constipation), new food sensitivities during stress, and mood swings or anxiety that coincide with digestive flare‑ups.
3. Can I heal gut trauma naturally at home?
Yes. Gentle strategies—like diaphragmatic breathing, self‑abdominal massage, somatic movement, and mindful eating—can help unlock stored tension. Pair these with a nourishing, anti‑inflammatory diet and you’ll support both your enteric nervous system and your body’s innate healing.
4. Which foods help release emotional trauma from the gut?
Focus on whole, gut‑soothing choices: bone broth or collagen for gut lining repair; fibrous vegetables and resistant starches to feed beneficial bacteria; omega‑3 rich foods (e.g., wild salmon, chia seeds); and fermented items like kimchi or kefir to replenish your microbiome.
5. How long does it take to release trauma stored in the gut?
Healing timelines vary, but many people notice shifts within 2–4 weeks of consistent practice. Deeper trauma may require 3–6 months of combined self‑care (breathwork, movement, nutrition) and professional support (e.g., somatic therapy or EMDR).
6. Should I see a therapist, a nutritionist, or both?
For best results, consider an integrative approach. A trauma‑informed therapist can guide you through embodied release techniques, while a nutritionist or functional medicine practitioner can help tailor your diet and supplements to rebuild gut health.